Case Report
Brachial Plexus Schwannoma: Report of 4 cases with Intralesional Enucleation

Jennette SY Chan* and Josephine WY Ip
Division of Hand and Foot Surgery, Department of Orthopaedics and Tramatology, The University of Hong Kong, Hong Kong*Address for Correspondence: Jennette SY Chan, Division of Hand and Foot Surgery, Department of Orthopaedics and Tramatology, The University of Hong Kong, Hong Kong, Email: [email protected]
Dates: Submitted: 03 October 2017; Approved: 28 December 2017; Published: 28 December 2017
How to cite this article: Chan JSY, Josephine WY Ip. Brachial Plexus Schwannoma: Report of 4 cases with Intralesional Enucleation. Arch Clin Exp Orthop. 2017; 1: 004-009. DOI: 10.29328/journal.aceo.1001002
Copyright Licence: © 2017 Chan JSY, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Brachial plexus tumours are rare. It comprises of only 5% of all tumours of upper limb [1]. The two most common brachial plexus region tumors are schwannomas and neurofibromas [2-4]. Both are benign and arise from the nerve sheath. XiaotianJia et al., published a large case series of 143 patients with primary brachial plexus tumors in 2016. In his series, there are 119 schwannoma and 12 neurofibromas [3]. Schwannomas are most frequently found in the head and neck region, which comprises 25% of all Schwannomas. There are only about 5% of schwannomas present as brachial plexus tumours [5].
The most common clinical presentation of primary brachial plexus tumor includes palpable mass, pain, numbness or paresthesias, weakness etc. [3-6], Brachial plexus schwannoma can present as neck mass, axillary mass, supraclavicular mass or apical lung mass [7-10]. On CT, most schwannomas are iso-dense relative to brain parenchyma. Calcification or areas of hemorrhage are rare and the enhancement pattern is typically homogeneous. On MRI, schwannomas are iso-intense to hypo-intense on T1-weighted MRI and enhance with gadolinium [11,12]. Malignant transformation of schwannoma is very rare, but it has been reported in literature [13]. Outcome of surgical removal of brachial plexus schwannoma has been reported to be satisfactory [14].
We report four cases of brachial plexus schwannoma with surgical removal managed in our centre from 2013 to 2016.
Methods
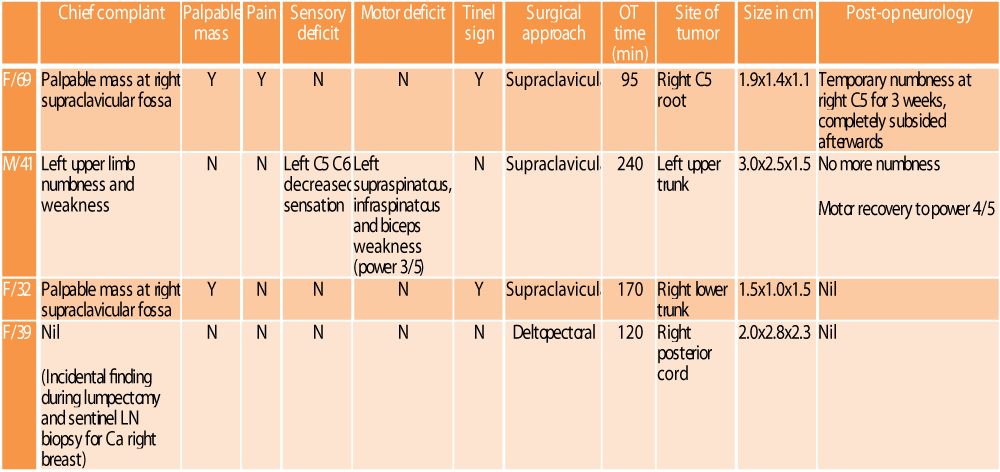
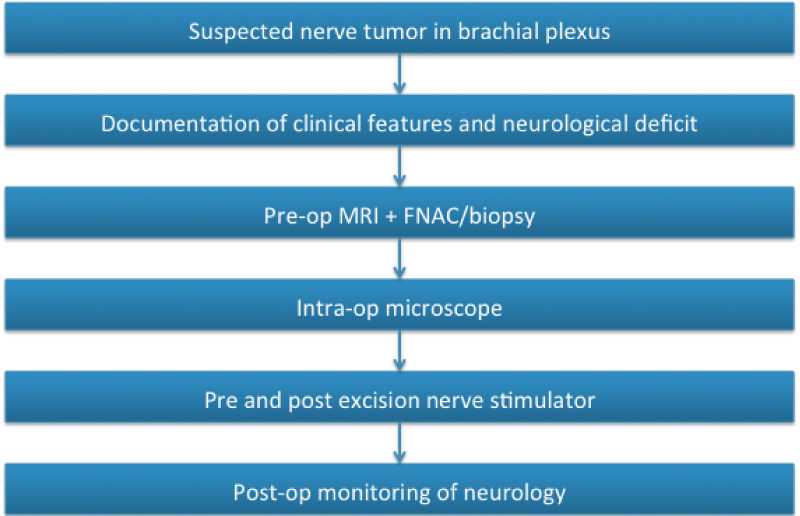
There were four cases of brachial plexus schwannoma managed operatively in our centre from 2013 to 2016. Pre-operatively, magnetic resonance imaging (MRI) and fine needle aspiration (FNA)/biopsy were performed. All the four cases had intranuclear enucleation done under general anesthesia. Microscope was used to assist the procedure intra-operatively. Pre and post excision of the tumor, nerve stimulator was used to confirm intact motor function of the nerve. At the site of enucleation, the nerve was wrapped with commercial anti-adhesive paper made of polylactic acid after removal of tumor. All the excised tumors had histopathological proof of schwannoma. There was no evidence of malignancy in all cases. The clinical information of the four cases was summarized in the following table 1.
Case 1
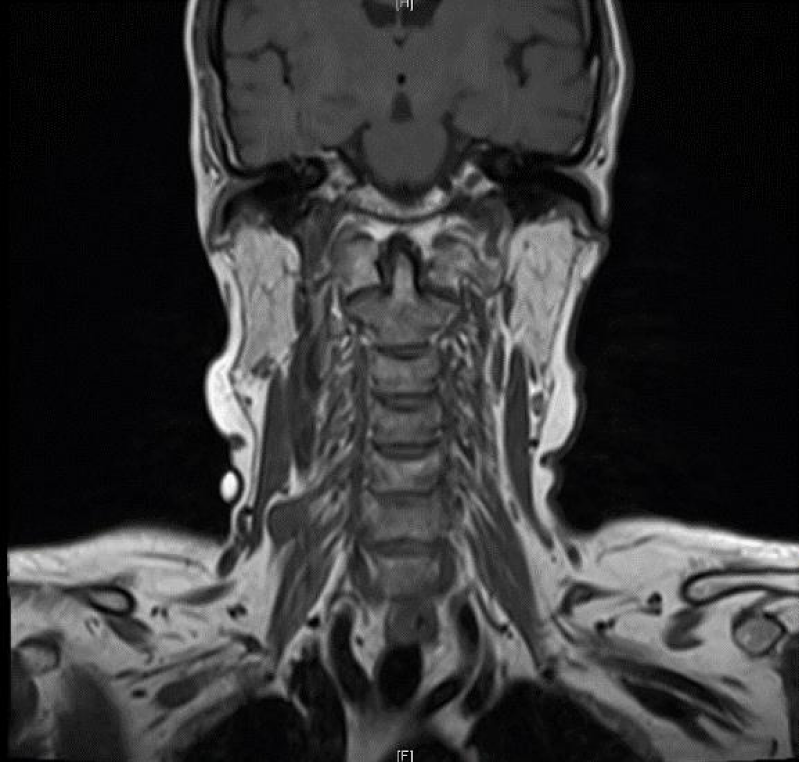
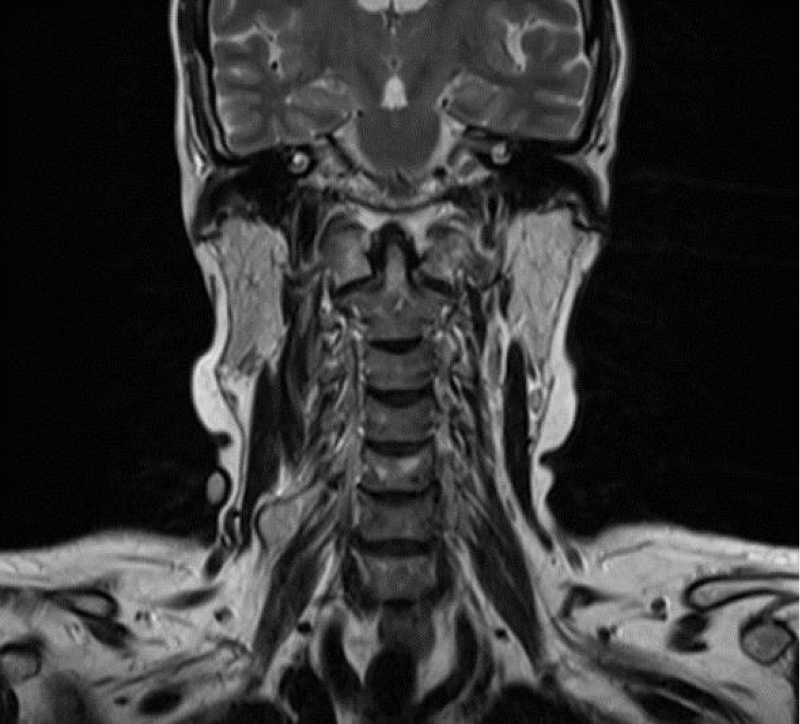
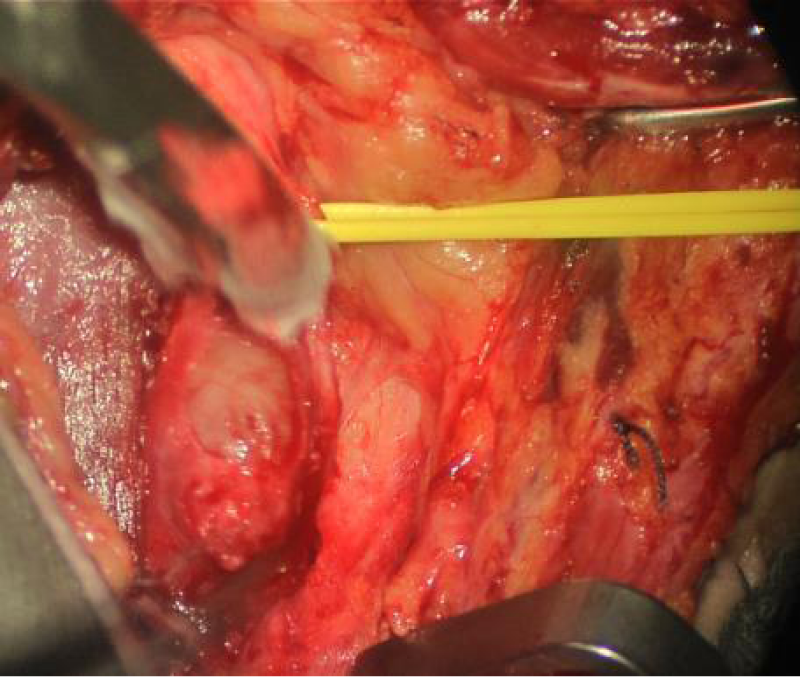
A 69 year-old lady complained of a painful palpable mass at her right supraclavicular fossa (Figure 1). There was no neurological deficit. Tinel sign was positive. MRI showed there was a well-defined homogenous T1 hypointense (Figure 2) and T2 hyperintense lesion at right C5 nerve root (Figure 3). Supraclavicular approach was used with a L-shaped incision at the lateral border of sternocleidomastoid muscle and upper border of clavicle (Figure 4). A 1.9x1.4x1.1cm tumor was surgically removed from right C5 nerve root (Figure 5). After the operation, there was temporary numbness at right C5 dermatome for 3 weeks. It completely subsided afterwards.
Case 2
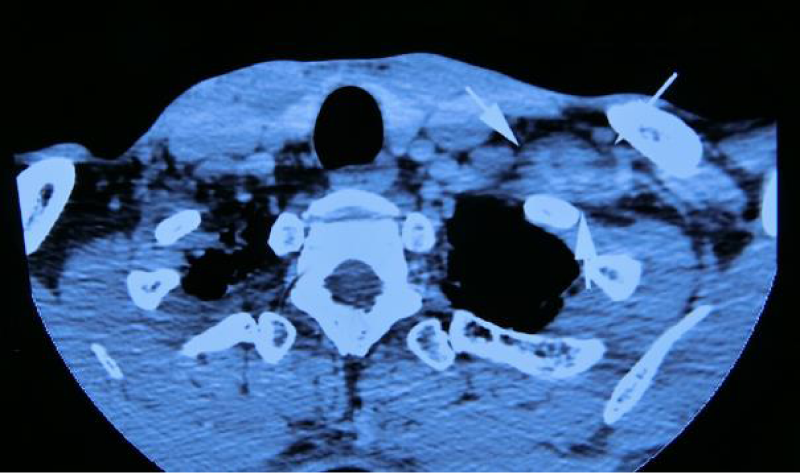
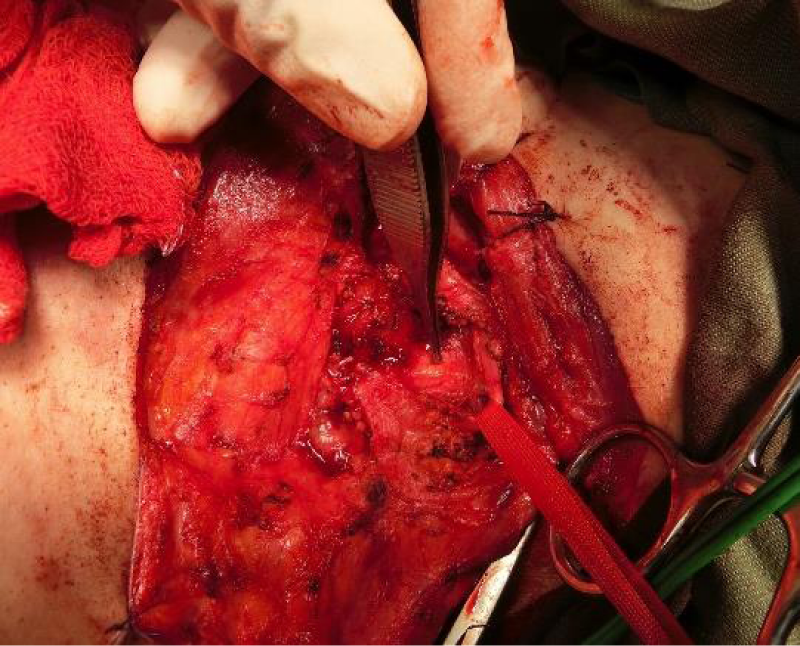
Patient was a 41 year-old male. He presented with left upper limb numbness and weakness. There was no palpable mass. Upon physical examination, there was decreased sensation at left C5 and C6 dermatome. There was also weakness at left supraspinatous, infraspinatous and biceps muscle with MRC grade 3/5. MRI found that there was a well-defined homogenous T1 hypointense and T2 hyperintense lesion (Figures 6,7) at upper trunk of left brachial plexus. Supraclavicular approach was used to remove the lesion (Figure 8). Post-operatively, there was no more upper limb numbness. The power of the involved muscle improved to MRC grade 4/5.
Case 3
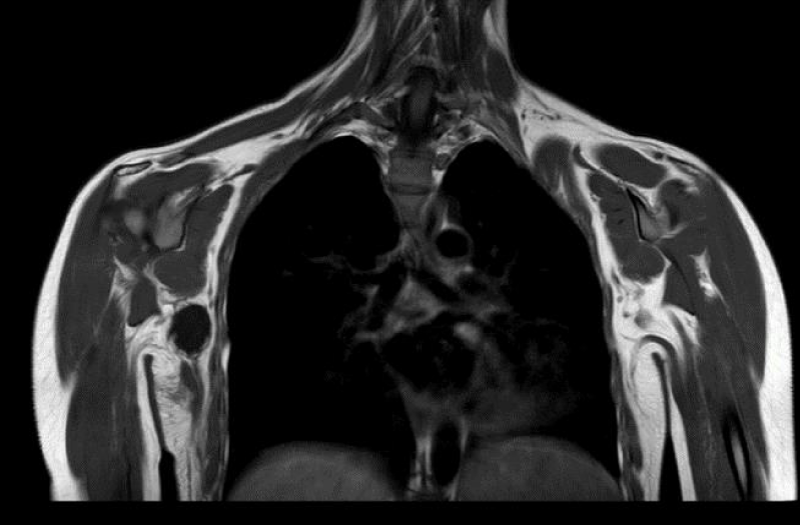
A 32 years-old lady complained of a palpable painless mass at her right supraclavicular fossa. Sensory and motor function was intact. There was positive Tinel sign. Pre-operative MRI scan showed typical feature of schwannoma (Figures 9,10). Supraclavicular approach was adopted for enucleation of lesion. There was a 1.5x1.0x1.5cm schwannoma at the upper trunk of right brachial plexus. No neurological deficit was found after the surgery.
Case 4
A 39 year-old lady had cancer of right breast. There was an incidental finding of an axillary mass during lumpectomy of right breast and sentinel lymph node biopsy surgery. Patient was asymptomatic. She was then referred to our team for further management. MRI and biopsy confirmed the mass was a brachial plexus schwannoma (Figures 11,12). Deltopectoral approach was used in this case (Figure 13). There was a 2.0x2.8x2.3cm lesion located at posterior cord of right brachial. Enucleation was performed. There was no neurological deficit after the operation.
Conclusion
We obtained similar clinical characteristics of brachial plexus schwannoma as those reported in litreture [3,4,6-10]. Brachial plexus schwannoma could be a painless or painful mass. Neurological deficit was not always present. The lesions were found at supraclavicular or axillary region. MRI was a valuable diagnostic tool [15]. In our cases, the MRI features of the tumors were consistent. It showed a well-defined homogenous lesion, hypointense in T1 weighted film and hyperintense in T2 weighted film.
Since the lesion is benign, the aim of surgery should be maximal debulking of tumor with minimal damage to normal nerve fibres. The described method of intralesional enucleation provided satisfactory outcome in all 4 cases. There was no irreversible neurological damage after the operation. With the mean follow-up period of 27 months, there was no evidence of recurrence of tumor. Our management pathway for brachial plexus schwannoma was summarized below (Table 2).
References
- Donner TR, Voorhies RM, Kline DG. Neural sheath tumours of major nerves. J Neurosurg. 1994; 81: 362-373. Ref.: https://goo.gl/ARsp5En
- Ganju A, Roosen N, Kline DG, Tiel RL. Outcomes in a consecutive series of 111 surgically treated plexal tumors: a review of the experience at the Louisiana State University Health Sciences Center. J Neurosurg. 2001; 95: 51-60. Ref.: https://goo.gl/AfoMu4
- Xiaotian Jia, Jianyun Yanga, Lin Chen, Cong Yu, Tadashi Kondo. Primary Brachial Plexus Tumors: Clinical Experiences of 143 Cases. Clin Neurol Neurosurg. 2016; 148: 91-95. Ref.: https://goo.gl/B8h2rn
- Devin K Blinder, Justin S Smith, Nicholas M Barbaro. Primary brachial plexus tumors: imaging, surgical, and pathological findings in 25 patients. Neurosurg Focus. 2004; 16: 1-6. Ref.: https://goo.gl/qvGjzX
- Huang JH, Samadani U, Zager EL. Brachial plexus region tumors: a review of their history, classification, surgical management, and outcomes. Neurosurg Q. 2003; 13: 151-161. Ref.: https://goo.gl/SWbSnS
- Lee HJ, Kim JH, Rhee SH, Gong HS, Baek GH. Is surgery for brachial plexus schwannomas safe and effective? Clinical Neurology and Neurosurgery. 2014; 148: 91-95. Ref.: https://goo.gl/JQStjw
- Kumar A, Akhtar S. Schwannoma of Brachial Plexus. Indian J Surg. 2011; 73: 80-81. Ref.: https://goo.gl/zp8pbv
- Rashid, Salahuddin O, Yousaf S, Qazi UA, Yousaf K. Schwannoma of the brachial plexus; report of two cases involving the C7 root. Journal of Brachial Plexus and Peripheral Nerve Injury. 2013; 8: 12. Ref.: https://goo.gl/j6KfNM
- Ahmadi A, Hirbod H, Cheraghipoor M, Izadi F. Schwannoma of the Brachial Plexus Presented as a Neck Mass: A Case Report and Review of the Literature. International Journal of Otolaryngology and Head Neck Surgery. 2015; 4: 104-107. Ref.: https://goo.gl/8agcBp
- Munireddy MV, Pavan BK, Bhaskaran A. Schwannoma of Brachial Plexus Presenting as Supraclavicular Mass: A Rare Presentation, Evaluation and its Management is a Challenge to Surgeons. Journal of Medical Science And clinical Research. 2017; 5: 26114-26117.
- Chung SY, Kim DI, Lee BH, Yoon PH, Jeon P, et al. Facial nerve schwannomas: CT and MR findings. Yonsei Med J. 1998; 39: 148-153. Ref.: https://goo.gl/u8Q5k3
- Bartolome A, González-Alenda J, Bartolomé MJ, Fraile E, Sánchez de las Matas I, et al. Study of the brachial plexus by magnetic resonance. Rev Neurol. 1998; 26: 983-988. Ref.: https://goo.gl/5aEzUN
- Nayler SJ, Leiman G, Omar T, Cooper K. Malignant transformation in a schwannoma. Histopathology. 1996; 2: 189-192. Ref.: https://goo.gl/EdmCP5
- Hyuk Jin Lee, Jeong Hwan Kim, Seung Hwan Rhee, Hyun Sik Gong, Goo Hyun Baek. Is Surgery for Brachial Plexus Schwannomas Safe and Effective? Clin Orthop Relat Res. 2014; 472: 1893-1898. Ref.: https://goo.gl/ZS65rs
- Prem A. Kumar, Biju Islary, Ramya Ramachandra, Thippeswamy Naik. Axillary Nerve Schwannoma: A Rare Case Report. Asian J Neurosurg. 2017; 12: 787-789. Ref.: https://goo.gl/vB76k1