More Information
Submitted: November 18, 2024 | Approved: November 23, 2024 | Published: November 25, 2024
How to cite this article: Wang S, Lu N, Li Y, Tu X, Chen A. Anterior Laparoscopic Approach Combined with Posterior Approach for Lumbosacral Neurolysis: A Case Report. Arch Clin Exp Orthop. 2024; 8(1): 010-013. Available from: https://dx.doi.org/10.29328/journal.aceo.1001020.
DOI: 10.29328/journal.aceo.1001020
Copyright Licence: © 2024 Wang S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Lumbosacral plexus injury; Laparoscope; Neurolysis
Anterior Laparoscopic Approach Combined with Posterior Approach for Lumbosacral Neurolysis: A Case Report
Sheng Wang1#, Nan Lu1#, Yongchuan Li1#, Xiaohuang Tu2* and Aimin Chen1*
1Department of Traumatic Orthopedics, Shanghai Fourth People’s Hospital, School of Medicine, Tongji University, Shanghai, 200434, China
2Department of Gastroenterology, Shanghai Fourth People’s Hospital, School of Medicine, Tongji University, Shanghai, 200434, China
#These authors contributed equally to the article
*Address for Correspondence: Aimin Chen, Department of Traumatic Orthopedics, Shanghai Fourth People’s Hospital, School of Medicine, Tongji University, Shanghai, 200434, China, Email: [email protected]
Xiaohuang Tu, Department of Gastroenterology, Shanghai Fourth People’s Hospital, School of Medicine, Tongji University, Shanghai, 200434, China, Email: [email protected]
Background and importance: Sacral fractures often lead to injuries of the lumbosacral nerve, which will cause tremendous damage to the patient’s motor and sensory functions. At present, the most commonly used surgical method is the posterior median approach, the extent and degree of neurolysis are often insufficient, so the effect of neurolysis is not well, and the functional recovery of patients after operation is often incomplete.
Clinical presentation: The patient was a 17-year-old male who accidentally fell from a height and landed on his hip. The main clinical feature of the patient was persistent radiating pain in the right lower extremity with right lower limb sensorimotor disorder. The results of the X-ray examination indicated a sacral fracture and a right pubic fracture. After the injury, the patient underwent pelvic internal fixation surgery within 72 hours. Then 6 months after the surgery, there was no significant improvement in right lower limb function, and the patient came to our hospital seeking treatment. Considering the severe lumbosacral plexus injury and the history of surgery, we performed an “Anterior surgery approach combined with posterior approach for lumbosacral neurolysis” for the patient, postoperative radiation pain disappeared completely, and there were significant improvements in the muscle strength of some muscles and sensory function.
Conclusion: The relaxation of the lumbosacral plexus is usually performed through a single surgical approach, which has great limitations in the effect of relaxation. Here, we demonstrate a case in which posterior lumbar incision and anterior laparoscopic lumbosacral plexus neurolysis can benefit the patient, the lumbosacral nerve was released to a great extent. We aim to bring this case to the attention of our worldwide neurosurgical colleagues and share our surgical approach to assist those who may encounter this case in the future.
Lumbosacral nerve injury is often caused by contusion, compression, and traction injury. Clinical experience reminds us that sacral fractures are usually associated with compression and injury of the lumbosacral plexus [1,2]. And when sacral fracture reduction and fixation are performed, this can lead to an exacerbation of nerve injury due to improper manipulation [3-5], which will severely affect the normal sensory and motor function of the patient. At this time, early surgical intervention and treatment are particularly important, it has been reported that neurologic deficits can be improved by up to 80% after surgical treatment [6]. Therefore, it is necessary to perform surgery in time.
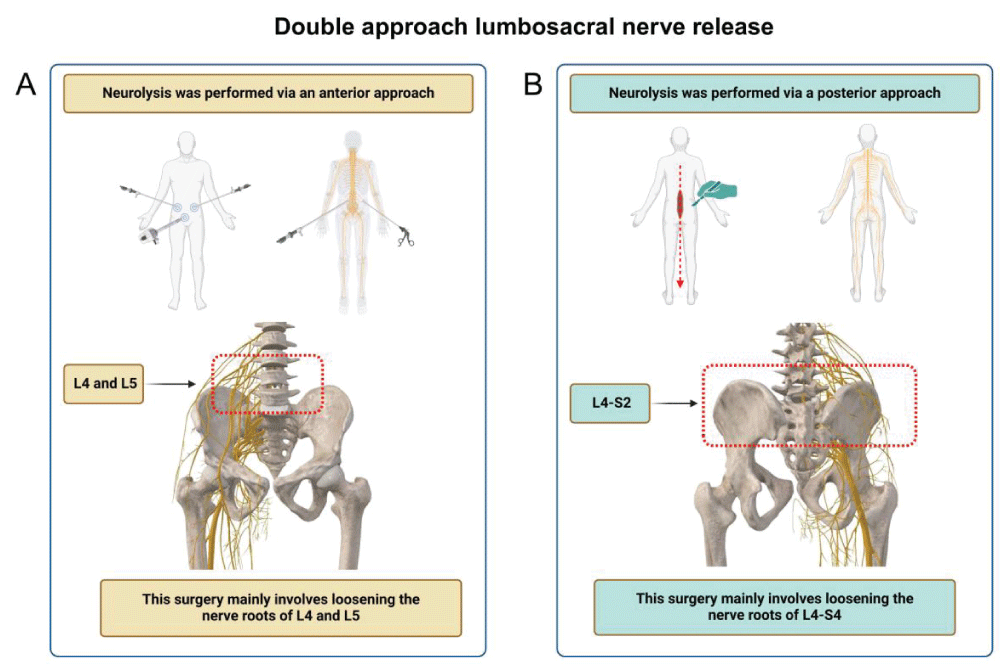
In terms of surgical methods, the most common one is expanded decompression of sacral foramina via the posterior approach. Although this surgical method is safe, it has certain limitations because it cannot directly view the presacral area [7,8]. In recent years, anterior neurolysis has been gradually accepted, and the surgical incision is often the lateral rectus abdominis. This kind of operation is convenient for L4 and L5 nerve root decompression, but relatively difficult for sacral nerve decompression [9,10]. Therefore, the combined treatment of anterior and posterior surgical approaches can bring better therapeutic effects. In order to minimize the patient’s injury as much as possible, we creatively adopted a laparoscopic-assisted anterior approach, combined with the conventional neurolysis of the posterior approach, and completed one case of neurolysis (Figure 1A,B). This operation is the first case in the world, which can not only ensure the effect of neurolysis, but also reduce the damage of the operation, and has high clinical application value.
Figure 1: Schematic diagram of dual-approach neurolysis. (A) Anterior approach neurolysis (Laparoscopic neurolysis), L4 and L5 were the main nerves released. (B) Posterior approach neurolysis, L4-S2 were the main nerves released.
A 17-year-old man accidentally fell from a height and landed on his hip. After the injury, the patient felt obvious pain in the sacrococcygeal region and right hip, and sensorimotor disorder of the right lower limb. An imaging examination showed a sacral fracture and a right pubic fracture. On the 3 days after injury, pelvic fracture open reduction and internal fixation surgery were performed. After 6 months of functional exercise and recovery, there was no significant improvement in the motor and sensory functions of the right lower limb.
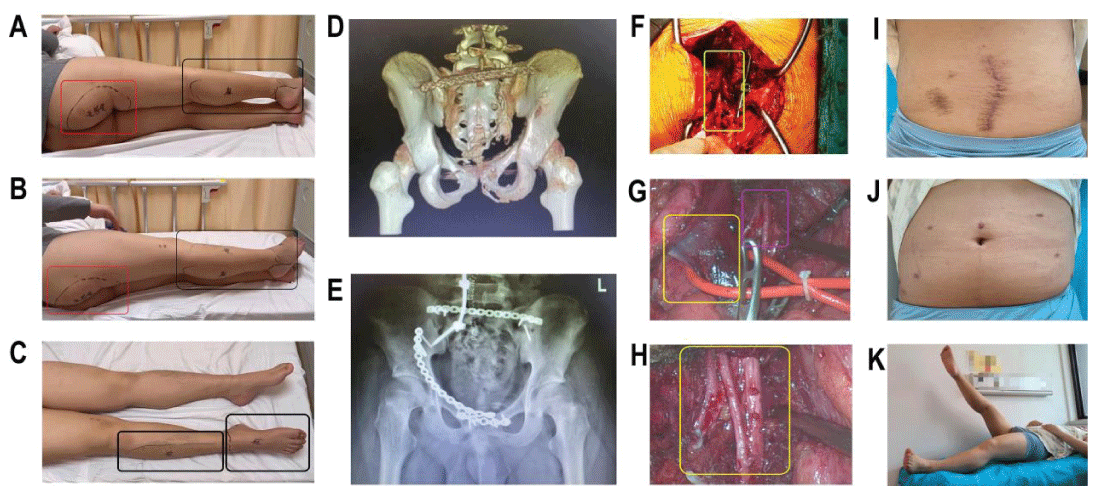
Then the patient came to our hospital for treatment, and the physical examination results showed that there were old surgical scars visible in the patient’s lumbosacral region and right inguinal region, with positive tenderness in the lumbosacral region. The left lower limb muscle strength of the patient is normal, while the right lower limb muscle strength is significantly reduced. Radiating pain was evident in the right lower limb. The right toe extension is at level 0, toe flexion is at level 0, right ankle dorsiflexion is at level 0, plantar flexion is at level 2, right knee extension is at level 3, flexion is at level 2, right hip flexion is at level 4, abduction is at level 3, and extension is at level 4. At the same time, the patient feels numbness in the skin around the right anus and perineum, as well as obvious numbness in the skin on the right buttocks, outer side of the right calf, and dorsal side of the right foot. Especially persistent radiating pain in the right lower limb, which causes great pain to the patient (Figure 2A-C).
Figure 2: The patient's preoperative evaluation and intraoperative neurolysis. (A-C) The area of sensory disturbance before operation, the area with the red border is the senseless area, and the area with the black border is the sensory numbness area. (D-E) X-ray and CT three-dimensional reconstruction before operation. (F) Posterior approach lumbosacral neurolysis, the yellow border area is the loosened nerve. (G) Laparoscopic exposure of the lumbar nerve, the yellow border area shows the iliac vessels and the purple border area is the lumbar nerve. (H) Laparoscopic exposure of the lumbar nerve, the yellow border area is the loosened nerve. (I and J) Six months after surgery, the abdominal and lumbar incisions recovered well. (K) Six months after surgery, the motor function of the patients was obviously improved.
The pelvic CT results indicate fractures of the pelvis and sacrum with internal fixation (Figure 2D-E). EMG results indicate severe injury to the sacral plexus nerve in the right lower limb. Considering that the patient has severe damage to the lumbosacral plexus and has a history of surgery, a single posterior or anterior approach for nerve release may not achieve the expected result. Therefore, we have decided to use the “dual approach lumbar sacral nerve release surgery” for the patient’s treatment. Considering that laparoscopic anterior surgery can preferentially reduce injury, the final surgical plan is “posterior lumbar incision and anterior laparoscopic lumbar-sacral plexus release surgery”.
Firstly, the patient is placed in a prone position and an incision is made along the posterior midline, to expose the right L4-S2 vertebral body. Decompression was performed on the right vertebral plate of L4~S2, and the results showed continuity of the L4~S2 nerves, but there was significant traction damage in this area. L5 and S1 become significantly thicker and purple at the sacral foramen, while S2 scars form. There was no response after stimulating L4-S2. Cut the outer membrane of the L4-S2 spinal nerve longitudinally and release the nerve (Figure 2F). The patient is placed in a supine split leg position, and a 10mm Troca is inserted into the abdominal cavity to establish pneumoperitoneum. Two Troc holes are placed on the left and right sides of the abdomen respectively. Enter the retroperitoneal area, ligate the vertebral body and the communicating branch of the retroperitoneal blood vessels, cut open the psoas major muscle, and enter the lumbar nerve root plane from the right side of the L4 and L5 vertebral bodies. Scars were observed around the nerve roots of the L4 and L5 spinal nerves during exploration. Provide sharp and blunt separation, release the nerve in the direction parallel to the nerve path, and release the L4 and L5 nerves to the lumbosacral nerve trunk, the iliac vessels were protected during the operation (Figure 2G,H). Finally, suture the retroperitoneal space and opening layer by layer. Through the double approach, the nerve segments in the root canal, spinal canal, and pelvic cavity were released, so that the compressed nerve was released to the greatest extent.
Postoperatively, the radiating pain of the patient’s lower limbs was significantly relieved. The patient was followed up 6 months after surgery, the patient’s surgical incision recovered well and the muscle strength of the patient’s right buttocks, thighs, and calves also showed significant improvement, the average muscle strength increased by about 1 grade. At the same time, the sensory impairment in the patient’s right thigh and right calf area has also been improved. However, the sensory and motor deficits of the right foot did not improve significantly (Figure 2I-K). In short, the patient benefits from the surgery, and there is a significant improvement in the sensory and movement function of the right lower limb.
For the treatment of sacral fracture combined with sacral plexus nerve injury, most scholars currently believe that sacral fracture combined with sacral plexus nerve injury requires the restoration of sacral anatomical structure and internal fixation, as well as nerve decompression and release [11-13]. In clinical practice, the nerve decompression and relaxation of many patients are not thorough enough, which will lead to incomplete postoperative functional recovery and greatly affect the effectiveness of the surgery. Therefore, choosing the appropriate nerve-release surgery method is extremely important.
In terms of nerve release surgery, some scholars believe that the risk of using the posterior approach for sacral foramen release surgery is relatively small, but this surgical method cannot effectively remove the displaced fracture block in the front. The main cause of sacral nerve symptoms is precisely the narrowing of the sacral foramen caused by the displaced bone block in the front, which compresses the nerves [14]. Based on this, some scholars choose the anterior approach to perform nerve decompression on patients. The more classic surgical method is the lateral rectus incision, which includes the exposure, exploration, decompression, and release of the lumbosacral plexus. The biggest advantage is that it can directly display the nerve roots of L4 and L5 in front of the sacrum and perform decompression under direct vision [9]. However, this surgery also has its own shortcomings. The abdominal incision increases the incidence of incisional hernia, and the probability of opening the peritoneum and small blood vessel bleeding can reach 4% [15]. Therefore, laparoscopic surgery, which is less damaging and safer, has been explored. Scholars have performed sacral ganglionectomy under laparoscopy to treat pelvic pain caused by endometriosis [16] and achieved good results.
In this case, the patient had undergone previous abdominal surgery, in which the patient’s abdominal anatomy had changed. Complications such as bleeding and organ damage may occur during routine anterior approach surgery because the anatomy is unclear. At the same time, complete lumbosacral neurolysis is necessary because the patient has significant sensory and motor deficits. Based on the above basic information about the patient and surgical experience, we combine the advantages of anterior and posterior surgery and use laparoscopy as a minimally invasive surgical method during anterior surgery to perform “dual approach lumbar sacral nerve release surgery” for the patient’s treatment. The patient’s lower limb function was sufficiently improved by surgery.
In summary, this dual approach lumbar surgery with laparoscopic assistance has the following two major advantages: Loosening effect is thorough, which can comprehensively release the damaged nerves and help patients recover their neurological function. Minimal trauma, laparoscopic release can reduce surgical trauma, reduce the occurrence of surgical complications, and shorten the postoperative recovery period of patients. This surgical method is the world’s first, ensuring the effectiveness of release while reducing the risk of injury. We hope that this surgery can be better applied to clinical patients and bring good news to patients with lumbar sacral nerve injury.
The surgical treatment of sacral nerve injury is very difficult, and patients often experience a decrease in lower limb motor and sensory function, which seriously affects their daily life and treatment. We report the first case of “dual approach lumbar sacral nerve release surgery” and achieved good surgical results. Our goal is to make this surgical method attract the attention of clinical workers and ultimately benefit more clinical patients.
Funding
This study was supported by Construction of Clinical Key Specialty of Hongkou District Health Committee in 2024 (HKLCZD2024B02, China) and Nature Science Foundation of China (82171371, China).
Ethical statement
The patient consented to the publication of the manuscript and signed the relevant documents.
- Allison DW, Verma A, Holman PJ, Huang M, Trask TW, Barber SM, et al. Transabdominal motor evoked potential neuromonitoring of lumbosacral spine surgery. The Spine Journal: official journal of the North American Spine Society. 2024;24(9):1660-1670. Available from: https://doi.org/10.1016/j.spinee.2024.04.029
- Wang S, Xia D, Song D, Lu N, Chen A. Could nerve transplantation be the future of this field: a bibliometric analysis about lumbosacral plexus injury. International journal of surgery (London, England). 2024;110(6):3734-3744. Available from: https://doi.org/10.1097/js9.0000000000001332
- Bellabarba C, Schildhauer TA, Vaccaro AR, Chapman JR. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine. 2006;31(11 Suppl):S80-8; discussion S104. Available from: https://doi.org/10.1097/01.brs.0000217949.31762.be
- Jones CB, Sietsema DL, Hoffmann MF. Can lumbopelvic fixation salvage unstable complex sacral fractures? Clinical orthopaedics and related research. 2012;470(8):2132-141. Available from: https://doi.org/10.1007/s11999-012-2273-z
- Schildhauer TA, Bellabarba C, Nork SE, Barei DP, Routt ML Jr., Chapman JR. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. Journal of orthopaedic trauma. 2006;20(7):447-457. Available from: https://doi.org/10.1097/00005131-200608000-00001
- Khan JM, Marquez-Lara A, Miller AN. Relationship of Sacral Fractures to Nerve Injury: Is the Denis Classification Still Accurate? Journal of orthopaedic trauma. 2017;31(4):181-184. Available from: https://doi.org/10.1097/bot.0000000000000772
- Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman JR, Schildhauer T, et al. Diagnosis and management of sacral spine fractures. Instructional course lectures. 2004;53:375-385. Available from: https://pubmed.ncbi.nlm.nih.gov/15116628/
- Matsumoto M, Watanabe K, Ishii K, Tsuji T, Takaishi H, Nakamura M, et al. Posterior decompression surgery for extraforaminal entrapment of the fifth lumbar spinal nerve at the lumbosacral junction. Journal of neurosurgery Spine. 2010;12(1):72-81. Available from: https://doi.org/10.3171/2009.7.spine09344
- Häckel S, Albers CE, Bastian JD, Hoppe S, Benneker LM, Keel MJB. Direct anterior decompression of L4 and L5 nerve root in sacral fractures using the pararectus approach: a technical note. Archives of orthopaedic and trauma surgery. 2020;140(3):343-351. Available from: https://doi.org/10.1007/s00402-019-03276-7
- Bureta CA, Yamamoto T, Ishidou Y, Abematsu M, Tominaga H, Horinouchi S, et al. Extraforaminal L5 Nerve Root Compression Caused by Intervertebral Osteophyte Accompanied by Lumbosacral Transitional Vertebra: A Case Treated by Anterior Approach. World neurosurgery. 2019;127:464-468. Available from: https://doi.org/10.1016/j.wneu.2019.04.104
- Chiodo A. Neurologic injury associated with pelvic trauma: radiology and electrodiagnosis evaluation and their relationships to pain and gait outcome. Archives of physical medicine and rehabilitation. 2007;88(9):1171-1176. Available from: https://doi.org/10.1016/j.apmr.2007.06.004
- Chen SY, Yang RL, Wu XC, Zhao DZ, Fu SP, Lin FQ, et al. Mesenchymal Stem Cell Transplantation: Neuroprotection and Nerve Regeneration After Spinal Cord Injury. Journal of inflammation research. 2023;16:4763-4776. Available from: https://doi.org/10.2147/jir.s428425
- Hasiba-Pappas S, Kamolz LP, Luze H, Nischwitz SP, Holzer-Geissler JCJ, Tuca AC, et al. Does Electrical Stimulation through Nerve Conduits Improve Peripheral Nerve Regeneration?-A Systematic Review. Journal of personalized medicine. 2023;13(3):414. Available from: https://doi.org/10.3390/jpm13030414
- Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clinical orthopaedics and related research. 1988;227:67-81. Available from: https://pubmed.ncbi.nlm.nih.gov/3338224/
- Keel MJB, Siebenrock KA, Tannast M, Bastian JD. The Pararectus Approach: A New Concept. JBJS essential surgical techniques. 2018;8(3):e21. Available from: https://doi.org/10.2106/jbjs.st.17.00060
- Chen FP, Soong YK. The efficacy and complications of laparoscopic presacral neurectomy in pelvic pain. Obstetrics and gynecology. 1997;90(6):974-977. Available from: https://doi.org/10.1016/s0029-7844(97)00484-5